Sarcoidosis
Published Web Location
https://doi.org/10.5070/D37s66b9xkMain Content
Sarcoidosis
Aimee L Leonard MD
Dermatology Online Journal 9(4): 40
From the Ronald O. Perelman Department of Dermatology, New York University
Abstract
A 54-year-old man presented with symmetric, bulbous, nodular enlargement of the nasal tip and alae nasi. At first inspection, the changes appeared to be consistent with rhinophyma, but a biopsy specimen showed noncaseating granulomata that were consistent with sarcoidosis. His laboratory, radiographic, and pulmonary function studies were consistent with systemic involvement.
Clinical summary
History.—A 54-year-old man had a 15-year history of an enlarged nose. The patient was referred to the Charles C. Harris Skin and Cancer Pavilion in October 2002, for laser surgery of presumed rhinophyma. The patient described a 15-year history of gradual nose thickening and enlargement, which was otherwise asymptomatic. His remaining skin was unaffected. He had received no previous medical treatment.
His medical problems included a past history of alcohol use and liver problems of unknown etiology. He had no prior history of rosacea. Review of systems disclosed myalgias as well as dyspnea on exertion when walking up stairs or walking more than a few blocks.
Physical Examination.—Symmetric, bulbous, nodular enlargement of the nasal tip and alae nasi was present. The remainder of the face was clear. Lacrimal sacs were normal. An ophthalmologic examination showed early cataracts.

|
|
| Figure 1 | Figure 2 |
|---|
Laboratory data.—A complete blood count was normal. Blood urea nitrogen was 20 mg/dL, creatinine 1.2 mg/dL, alanine aminotransferase 91 U/L, aspartate aminotransferase 93 U/L, alkaline phosphatase 170 U/L, creatinine phosphokinase 100 mU/ml, aldolase 8.1 U/L, and angiotensin converting enzyme 121 U/L. Hepatitis B antigen and hepatitis C antibody were negative. A chest radiograph detected no evidence of interstitial disease or hilar adenopathy. Pulmonary function tests showed hypoxemia and a restrictive pattern of pulmonary impairment. An echocardiogram showed moderate left atrial dilatation, apical hypokinesis, and a minimally decreased ejection fraction.
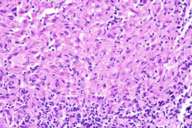
Histopathology.—There is a dermal, granulomatous inflammation composed of predominantly mono- and a few multinucleated epithelioid macrophages that have large vesicular nuclei and inconspicuous nucleoli and a moderate amount of eosinophilic cytoplasm. Macrophages are surrounded by a few small lymphocytes. A periodic acid-Schiff stain failed to show hyphae, and a Fite stain is negative for mycobacterium.
Diagnosis.—Sarcoidosis.
Comment.—Sarcoidosis is a systemic disease of unknown etiology that is characterized by noncaseating granulomatous inflammation of various organs. Pulmonary disease is the most common manifestation and affects nearly all patients [1]. Cutaneous involvement occurs in approximately 25 percent of cases [1]. Sarcoidosis remains a diagnosis of exclusion, and there are no definitive diagnostic blood, skin, or radiologic tests specific for the disorder.
The incidence of nose and paranasal sinus involvement with sarcoidosis is approximately 1 percent [2]. However, isolated nasal cutaneous involvement is much more uncommon and accounts for only 0.3 percent of patients [2]. When associated with underlying sinonasal mucosal lesions, patients can experience epistaxis, nasal congestion, polyps, rhinorrhea, and nasal crusts [2]. Complications may include septal perforation [3].
Nasal lesions of sarcoidosis are classically described as lupus pernio, which occurs as smooth, firm, shiny, indurated, red-to-violaceous plaques on the nose, lips, cheeks, and ears [4]. This case is unusual in that the cutaneous manifestations are bulbous nodules on the nose that resemble rhinophyma. One case of sarcoidosis mimicking rhinophyma has previously been reported. In that patient, a beneficial response to treatment with intralesional glucocorticoid injections was observed [5].
In addition to intralesional glucocorticoids, cutaneous nasal lesions of sarcoidosis have been treated successfully with high-potency topical [6] and systemic glucocorticoids [4]. Pulsed-dye lasers have been used for isolated lesions on the face. Although cosmetic improvement is achieved, the underlying process is not affected as the presence of sarcoidal granulomas persists [7]. For more widespread or recalcitrant disease, antimalarial agents, methotrexate, allopurinal, retinoids, infliximab, and thalidomide have demonstrated efficacy, although little comparative data on these treatments exist [1, 4, 8, 9].
References
1. Newman LS, et al. Sarcoidosis. N Engl J Med 336:1224, 1997.2. McCaffrey TV, McDonald TJ. Sarcoidosis of the nose and paranasal sinuses. Laryngoscope 93:1281, 1983.
3. Baum ED, et al. Sarcoidosis with nasal obstruction and septal perforation. Ear Nose Throat J 77:896, 1998.
4. English JC, et al. Sarcoidosis. J Am Acad Dermatol 44:725, 2001.
5. Goldenberg JD, et al. Sarcoidosis of the external nose mimicking rhinophyma: Case report and review of the literature. Ann Otol Rhinol Laryngol 107:514, 1998.
6. Khatri KA, et al. Lupus pernio: Successful treatment with a potent topical steroid. Arch Dermatol 131:617, 1995.
7. Cliff S, et al. The successful treatment of lupus pernio with the flashlamp pulsed dye laser. J Cutan Laser Ther 1:49, 1999.
8. Baughman RP, Lower EE. Infliximab for refractory sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis 18:133, 2001.
9. Carlesimo M, et al. Treatment of cutaneous and pulmonary sarcoidosis with thalidomide. J Am Acad Dermatol 32:866, 1995.
© 2003 Dermatology Online Journal

